This article first appeared on Bloomberg.com
As the number of new Covid-19 cases each day begins to slow in parts of the U.S. and states consider rolling back social-distancing measures, a huge unknown remains: Who has become immune to the disease — and for how long?
When the body’s immune system encounters a virus, it gets to work producing antibodies that can recognize a particular virus and attack it. And it’s commonly thought that once a person catches a virus, immunity makes it impossible to get sick from the same one again.
But it’s more complicated than that. Immunity is a spectrum. Some viruses result in life-long protection, such as those that cause chickenpox and measles. On the other end of that spectrum, human immunodeficiency virus, or HIV, doesn’t usually provide any protective shield.
When it comes to SARS-CoV-2, the virus that causes Covid-19, little is known yet about the body’s immune response to an infection, said George Rutherford, the head of infectious disease and global epidemiology at the University of California San Francisco. “That’s something that’s going to take a while to figure out.”
Understanding the level of viral immunity in survivors of Covid-19 will prove key in making decisions about how and when to lift restrictions. Tests that measure antibodies to the virus have been touted as a major part of efforts to restart the economy and get people back to work. New York state has approved an antibody test and plans to use it widely. Anthony Fauci, the leading U.S. infectious-disease expert, has suggested a future in which “certificates of immunity" would be required for returning workers.
But all these ideas may be getting ahead of themselves. Researchers first need to answer two key questions: How long do antibodies to SARS-CoV-2 remain in the body, and for how long do they prevent reinfection, if at all?
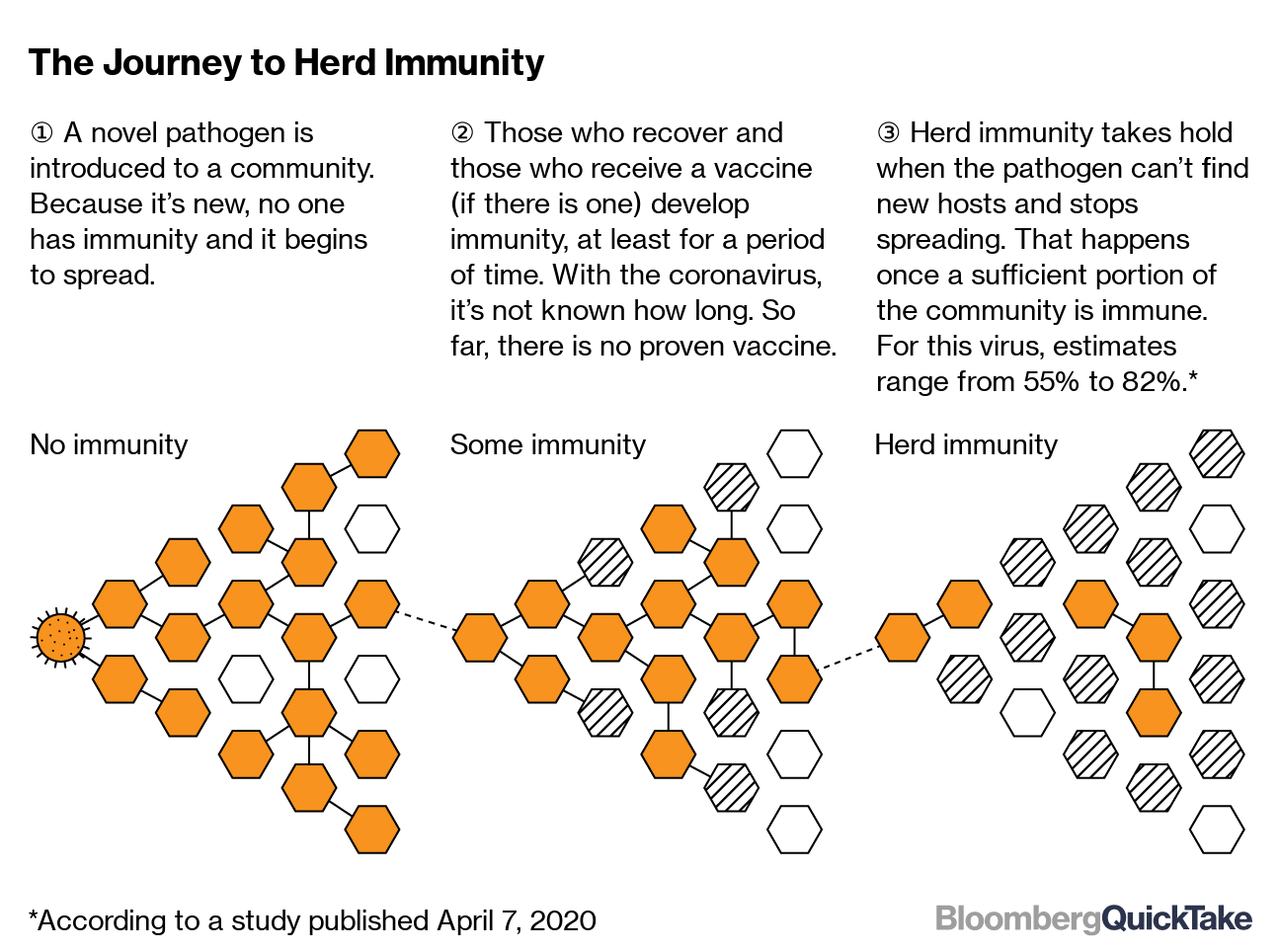
Rutherford said ideally, SARS-CoV-2 will be similar to viruses such as the one for rubeola that causes measles and triggers life-long immunity. In such a scenario, the virus eventually would stop spreading — what’s known as herd immunity.
“This is the hope for Covid-19,” Rutherford said.
But for now, that’s all it is: a hope. That’s because immunity is a particularly complicated question when it comes to coronaviruses, a class of viruses that includes SARS and MERS as well as seasonal coronaviruses that cause illnesses such as the common cold. They are named for the crown-like spiked proteins that allow them to attach to their cellular hosts.
“There is no proof at this point that the development of an antibody response will be protective,” said David Walt, a professor of pathology at Harvard Medical School and Brigham and Women’s Hospital in Boston. “There is no evidence yet that people can’t be reinfected with the virus.”
Studies of SARS and MERS, which are closely related to SARS-CoV-2, have suggested limits to the body’s immune response. One 2007 report on SARS demonstrated that its antibodies dissipated after an average of two years, making patients potentially vulnerable to reinfection. A study of MERS found antibodies tended to stick around for a bit longer, but not in everyone. And neither study demonstrated whether the presence of antibodies was protection against re-infection.
“The most similar virus to this shows there is not a protracted immune response,” Walt said.
Evidence from earlier studies also suggests having a coronavirus once does not make someone totally immune in the future. In 1984, for example, U.K. researchers infected human volunteers with a seasonal virus and then inoculated them a year later to test whether they had become immune. Those who were exposed to the exact same strain of the virus did not get sick, but some among those exposed to a slightly different strain still developed cold symptoms.
Exposure to the virus, researchers concluded, conferred only “partial immunity.” Another study published in 1990 found that in some people, the levels of antibodies to the virus declined so much over the course of a year that even exposure to the same strain didn’t necessarily prevent a second infection.
Complicating matters, not all antibodies are created equal. Only so-called “neutralizing” ones reduce or prevent infection by binding to a virus. Other types of antibodies are able to recognize a pathogen but not bind to it.
There is some recent, hopeful evidence that SARS-CoV-2 triggers the production of the neutralizing antibodies, Walt said. For example, blood-plasma transfusions from people who have recovered from the novel coronavirus at least appear to have a positive impact on Covid-19 patients in critical condition. Many hospitals have begun employing this treatment, and studies of it are underway.
But it isn’t clear how long these antibodies offer protection. Research out of South Korea’s Centers for Disease Control and Prevention reported that 91 infected patients tested negative for the virus and then later tested positive again. This could have a number of causes, including false negative results or continued shedding of virus fragments even after someone has recovered and the virus is no longer active in their body.
Another preliminary study out of Shanghai found that some patients had “no detectable antibody response” while others had a very high response. This week, World Health Organization officials said it’s unclear whether recovered coronavirus patients are immune to a second infection.
“With regards to recovery and then re-infection, I believe we do not have the answers to that. That is an unknown,” Mike Ryan, executive director of WHO’s emergencies programs, said at a press conference on Monday.
To better understand SARS-CoV-2 immunity, researchers will need to study the progress of the disease in many people over time, taking several samples from the same individuals. How long that will take is still open to much debate.
UCSF’s Rutherford says evidence suggests most people probably will have some immune response to SARS-CoV-2. Depending on how long that immunity lasts, seasonal vaccines or occasional boosters, as for tetanus, may be required.
“If we can get enough people immune in the population, this could die out,” he said. “It just goes back into bats or wherever it came from.”
